#covid 19 vaccination drive
Explore tagged Tumblr posts
Text
Jharkhand CM Links Covid Vaccine to Recruitment Deaths
Soren alleges ‘defective’ doses still causing fatalities; BJP rejects claims Jharkhand Chief Minister Hemant Soren stirs controversy by linking Covid-19 vaccine to recent deaths during constable recruitment tests. RANCHI – Jharkhand Chief Minister Hemant Soren has alleged that ‘defective’ Covid-19 vaccine doses administered during the pandemic may be responsible for recent deaths during constable…
#Assam-Jharkhand CM dispute#राज्य#BJP-JMM political clash#Constable recruitment deaths Jharkhand#Covid-19 vaccine safety debate#Hemant Soren vaccine allegations#Jharkhand Covid vaccine controversy#Jharkhand government stability#Jharkhand recruitment drive suspension#Jharkhand women welfare scheme#JMMSY scheme Jharkhand#state
0 notes
Text
Things Biden and the Democrats did, this week #25
June 28-July 5 2024
The Department of Labor's Occupational Safety and Health Administration (OSHA). Is putting forward the first ever federal safety regulation to protect worker's from excessive heat in the workplace. As climate change has caused extreme heat events to become more common work place deaths have risen from an average of 32 heat related deaths between 1992 and 2019 to 43 in 2022. The rules if finalized would require employers to provide drinking water and cool break areas at 80 degrees and at 90 degrees have mandatory 15-minute breaks every two hours and be monitored for signs of heat illness. This would effect an estimated 36 million workers.
The Federal Emergency Management Agency announced $1 Billion for 656 projects across the country aimed at helping local communities combat climate change fueled disasters like flooding and extreme heat. Some of the projects include $50 Million to Philadelphia for a stormwater pump station and combating flooding, and a grant to build Shaded bus shelters in Washington, D.C.
The Department of Transportation announced thanks to efforts by the Biden Administration flight cancellations at the lowest they've been in a decade. At just 1.4% for the year so far. Transportation Secretary Pete Buttigieg credited the Department's new rules requiring automatic refunds for any cancellations or undue delays as driving the good numbers as well as the investment of $25 billion in airport infrastructure that was in the Bipartisan Infrastructure Law.
The Department of Transportation announced $600 million in the 3rd round of funding to reconnect communities. Many communities have been divided by highways and other Infrastructure projects over the years. Most often effecting racial minority and poor areas. The Biden Administration is dedicated to addressing these injustices and helping reconnect communities split for decades. This funding round will see Atlanta’s Southside Communities reconnected as well as a redesign for Birmingham’s Black Main Street, reconnecting a community split by Interstate 65 in the 1960s.
The Biden Administration approved its 9th offshore wind power project. About 9 miles off the coast of New Jersey the planned wind farm will generated 2,800 megawatts of electricity, enough to power almost a million homes with totally clear power. This will bring the total amount of clean wind power generated by projects approved by the Biden Administration to 13 gigawatts. The Administration's climate goal is to generate 30 gigawatts from wind.
The Biden Administration announced funding for 12 new Regional Technology and Innovation Hubs. The $504 million dollars will go to supporting tech hubs in, Colorado, Montana, Indiana, Illinois, Nevada, New York, New Hampshire, South Carolina, Florida, Ohio, Oklahoma, and Wisconsin. These tech hubs together with 31 already announced and funded will support high tech manufacturing jobs, as well as training for 21st century jobs for millions of American workers.
HHS announced over $200 million to support improved care for older Americans, particularly those with Alzheimer’s and related dementias. The money is focused on training primary care physicians, nurse practitioners, and other health care clinicians in best practices in elder and dementia care, as well as seeking to integrate geriatric training into primary care. It also will support ways that families and other non-medical care givers can be educated to give support to aging people.
HHS announced $176 million to help support the development of a mRNA-based pandemic influenza vaccine. As part of the government's efforts to be ready before the next major pandemic it funds and supports new vaccine's to try to predict the next major pandemic. Moderna is working on an mRNA vaccine, much like the Covid-19, vaccine focused on the H5 and H7 avian influenza viruses, which experts fear could spread to humans and cause a Covid like event.
789 notes
·
View notes
Text
The danger is clear and present: COVID isn’t merely a respiratory illness; it’s a multi-dimensional threat impacting brain function, attacking almost all of the body’s organs, producing elevated risks of all kinds, and weakening our ability to fight off other diseases. Reinfections are thought to produce cumulative risks, and Long COVID is on the rise. Unfortunately, Long COVID is now being considered a long-term chronic illness — something many people will never fully recover from. Dr. Phillip Alvelda, a former program manager in DARPA’s Biological Technologies Office that pioneered the synthetic biology industry and the development of mRNA vaccine technology, is the founder of Medio Labs, a COVID diagnostic testing company. He has stepped forward as a strong critic of government COVID management, accusing health agencies of inadequacy and even deception. Alvelda is pushing for accountability and immediate action to tackle Long COVID and fend off future pandemics with stronger public health strategies. Contrary to public belief, he warns, COVID is not like the flu. New variants evolve much faster, making annual shots inadequate. He believes that if things continue as they are, with new COVID variants emerging and reinfections happening rapidly, the majority of Americans may eventually grapple with some form of Long COVID. Let’s repeat that: At the current rate of infection, most Americans may get Long COVID.
[...]
LP: A recent JAMA study found that US adults with Long COVID are more prone to depression and anxiety – and they’re struggling to afford treatment. Given the virus’s impact on the brain, I guess the link to mental health issues isn’t surprising. PA: There are all kinds of weird things going on that could be related to COVID’s cognitive effects. I’ll give you an example. We’ve noticed since the start of the pandemic that accidents are increasing. A report published by TRIP, a transportation research nonprofit, found that traffic fatalities in California increased by 22% from 2019 to 2022. They also found the likelihood of being killed in a traffic crash increased by 28% over that period. Other data, like studies from the National Highway Traffic Safety Administration, came to similar conclusions, reporting that traffic fatalities hit a 16-year high across the country in 2021. The TRIP report also looked at traffic fatalities on a national level and found that traffic fatalities increased by 19%. LP: What role might COVID play? PA: Research points to the various ways COVID attacks the brain. Some people who have been infected have suffered motor control damage, and that could be a factor in car crashes. News is beginning to emerge about other ways COVID impacts driving. For example, in Ireland, a driver’s COVID-related brain fog was linked to a crash that killed an elderly couple. Damage from COVID could be affecting people who are flying our planes, too. We’ve had pilots that had to quit because they couldn’t control the airplanes anymore. We know that medical events among U.S. military pilots were shown to have risen over 1,700% from 2019 to 2022, which the Pentagon attributes to the virus.
[...]
LP: You’ve criticized the track record of the CDC and the WHO – particularly their stubborn denial that COVID is airborne. PA: They knew the dangers of airborne transmission but refused to admit it for too long. They were warned repeatedly by scientists who studied aerosols. They instituted protections for themselves and for their kids against airborne transmission, but they didn’t tell the rest of us to do that.
[...]
LP: How would you grade Biden on how he’s handled the pandemic? PA: I’d give him an F. In some ways, he fails worse than Trump because more people have actually died from COVID on his watch than on Trump’s, though blame has to be shared with Republican governors and legislators who picked ideological fights opposing things like responsible masking, testing, vaccination, and ventilation improvements for partisan reasons. Biden’s administration has continued to promote the false idea that the vaccine is all that is needed, perpetuating the notion that the pandemic is over and you don’t need to do anything about it. Biden stopped the funding for surveillance and he stopped the funding for renewing vaccine advancement research. Trump allowed 400,000 people to die unnecessarily. The Biden administration policies have allowed more than 800,000 to 900,000 and counting.
[...]
LP: The situation with bird flu is certainly getting more concerning with the CDC confirming that a third person in the U.S. has tested positive after being exposed to infected cows. PA: Unfortunately, we’re repeating many of the same mistakes because we now know that the bird flu has made the jump to several species. The most important one now, of course, is the dairy cows. The dairy farmers have been refusing to let the government come in and inspect and test the cows. A team from Ohio State tested milk from a supermarket and found that 50% of the milk they tested was positive for bird flu viral particles.
[...]
PA: There’s a serious risk now in allowing the virus to freely evolve within the cow population. Each cow acts as a breeding ground for countless genetic mutations, potentially leading to strains capable of jumping to other species. If any of those countless genetic experiments within each cow prove successful in developing a strain transmissible to humans, we could face another pandemic – only this one could have a 58% death rate. Did you see the movie “Contagion?” It was remarkably accurate in its apocalyptic nature. And that virus only had a 20% death rate. If the bird flu makes the jump to human-to-human transition with even half of its current lethality, that would be disastrous.
#sars cov 2#covid 19#h5n1#bird flu#articles#long covid is def a global issue not just for those in the us and most countries aren't doing much better#regardless of how much lower the mortality rate for h5n1 may or may not become if/when it becomes transmissible between humans#having bird flu infect a population the majority of whose immune system has been decimated by sars2#to the point where the average person seems to have a hard time fighting off the common cold etc...#(see the stats of whooping cough/pertussis and how they're off the CHARTS this yr in the uk and aus compared to previous yrs?#in qld average no of cases was 242 over prev 4 yrs - there have been /3783/ diagnosed as of june 9 this yr and that's just in one state.#there's a severe shortage of meds for kids in aus bc of the demand and some parents visit +10 pharmacies w/o any luck)#well.#let's just say that i miss the days when ph orgs etc adhered to the precautionary principle and were criticised for 'overreacting'#bc nothing overly terrible happened in the end (often thanks to their so-called 'overreaction')#now to simply acknowledge the reality of an obviously worsening situation is to be accused of 'fearmongering'#🤷♂️#also putting long covid and bird flu aside for a sec:#one of the wildest things that everyone seems to overlook that conor browne and others on twt have been saying for yrs#is that the effects of the covid pandemic extend far beyond the direct impacts of being infected by the virus itself#we know sars2 rips apart immune system+attacks organs. that in effect makes one more susceptible to other viruses/bacterial infections etc#that in turn creates increased demand for healthcare services for all kinds of carers and medications#modern medicine and technology allows us to provide often effective and necessary treatment for all kinds of ailments#but what if there's not enough to go around? what happens when the demand is so high that it can't be provided fast enough -- or at all?#(that's assuming you can even afford it)#what happens when doctors and nurses and other healthcare workers keep quitting due to burnout from increased patients and/or illness#because they themselves do not live in a separate reality and are not any more sheltered from the effects of constant infection/reinfection#of sars2 and increased susceptibility to other illnesses/diseases than the rest of the world?#this is the 'new normal' that's being cultivated (the effects of which are already blatantly obvious if you're paying attention)#and importantly: it. doesn't. have. to. be. this. way.
283 notes
·
View notes
Text
The Weather
In the US, 41 out of 54 states and territories are at high or very high COVID wastewater levels as of 1/18/2024. Ten states and territories have no data available. It’s important to note that levels of “moderate,” “low,” or “minimal” do not necessarily indicate a low risk of COVID exposure in our daily lives. Viral spread is still ongoing even if at lower levels, and precautions are warranted to protect ourselves and others.

Looking at the CDC’s national and regional wastewater data over time, we continue to see “Very High” levels nationally. It’s important to note that the last two weeks are provisional data, indicated by a gray shaded area on the graph, meaning that those values can change as additional wastewater sites report data.
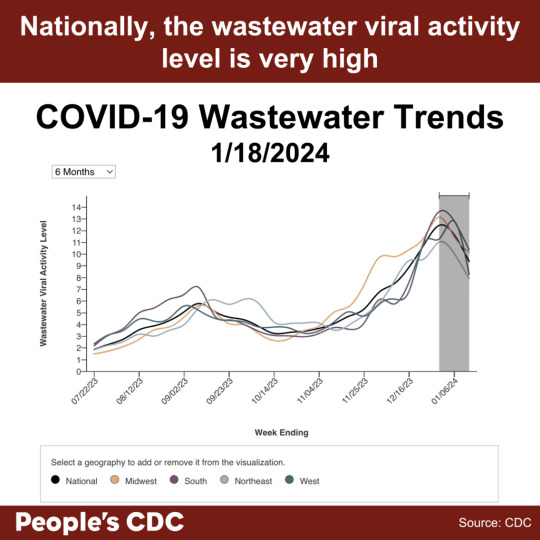
Although wastewater data does not provide the same level of detail as previous PCR-based testing data, wastewater monitoring is an important ongoing resource to inform us about the current COVID situation. While the provisional data tentatively shows a downward trend this week, time will tell whether this is a true decrease in the final data. A downward trend does not mean continued decreases are guaranteed or that protections should be relaxed. Multilayered protections help drive COVID spread lower, and relaxing protections can lead to a resurgence of viral spread.
Visit the CDC’s State and Territory Trends page to see available wastewater testing near you, including the number of wastewater sites reporting. Write your elected officials to let them know you want to keep and expand wastewater testing in your area and nationally.
Wins
In November 2023, the CDC’s Healthcare Infection Control Practices Advisory Committee (HICPAC) passed a series of draft proposals that will further weaken already insufficient protocols employed within healthcare settings. HICPAC refuses to reckon with the airborne nature of infectious diseases such as SARS-CoV-2, and does not propose crucial measures such as universal masking with well-fitted respirators, isolation periods, and ventilation. The People’s CDC has penned a letter to the ACLU alerting them of HICPAC’s irresponsible decisions, and the ramifications associated with them. We hope that by working together with the ACLU, we can implement public advocacy and legal actions in order to tackle this critical issue.
You can read the full letter here.
Johns Hopkins reinstated healthcare masking on 1/12/2024, in response to high respiratory virus levels. As with many other healthcare systems and public health departments that have restored healthcare masking when facing public pressure, we hope that universal masking can become a standard of care rather than a short term response to a surge. See “Take Action” below for more information.
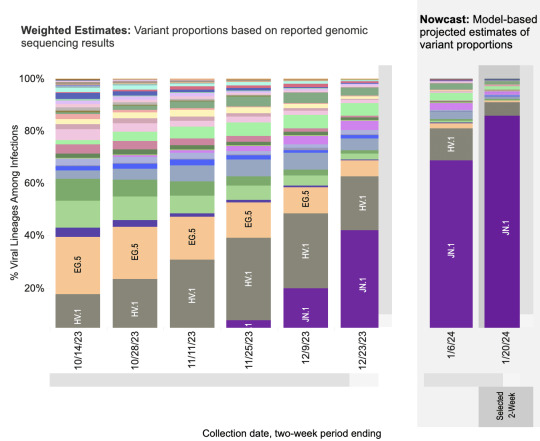
Variants
JN.1, now the most prominent variant in the United States, is estimated to account for 85.7% of circulating variants by 1/20/2024. HV.1 is expected to drop to 5.3%, and all other variants are estimated to make up less than 2% each. Although ongoing viral spread allows opportunities for new variants to emerge, the latest 2023-2024 COVID vaccine boosters, COVID tests, and COVID treatments are still expected to be effective for JN.1.
Current updated booster uptake is low (as of January 19, 2024, the CDC reports that only 21.5% of adults and 11% of children have received it). It is not too late to get the updated booster, and to protect yourself against the latest variant!
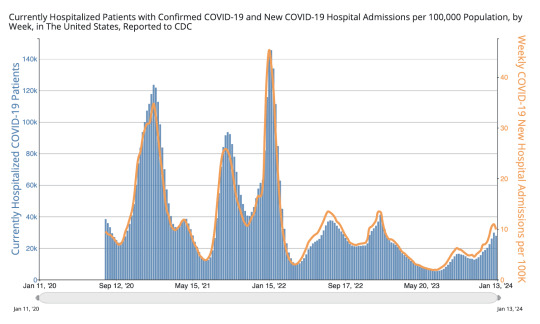
Hospitalizations
In the most recent week (ending January 13, 2024), we see a slight downward trend in new hospital admissions, currently at 32,861. We see a similar slight downtick in currently hospitalized patients with COVID , at 27,879. This most recent week shows a slight decrease in hospitalizations, although it is too soon to say whether hospitalizations for the current surge have passed their peak. Hospitals continue to be overwhelmed. The data also lacks information on hospital-acquired infections. We urge you to continue taking stringent precautions, such as donning a well-fitting respirator (e.g., N95, KN95) in all indoor spaces–and especially in healthcare settings.
Long COVID
Amid ongoing advocacy by Long COVID groups, the US Senate Committee on Health, Education, Labor, and Pensions (HELP) held a committee hearing on “Addressing Long COVID: Advancing Research and Improving Patient Care.” The hearing included testimony from three Long COVID patients and four Long COVID physicians and researchers, bringing much-needed attention to the urgent need for funding for Long COVID research and treatments, and to the need for improved access to care for Long COVID patients. We recognize the community care modeled by some of the panelists and attendees who wore masks for the hearing, and we wish the senators on the committee would mask up as well.
Take Action
Write your elected officials to let them know that Long COVID impacts all of us, and that we need ongoing support for Long COVID research and clinical care. Ask Senators to support bill S.2560, the Long COVID Support Act. Ask Representatives to support bills HR.1114 (Long COVID RECOVERY NOW Act) and HR.3258 (TREAT Long COVID Act).
Although some healthcare settings have reinstated masking in response to high COVID levels along with high respiratory virus activity, ongoing pressure is needed to restore, keep, and expand masking broadly. Use our letter template and toolkit to call or write your elected officials in support of healthcare masking.
Want to do more to support healthcare masking? Consider starting, sharing, or joining a local campaign. Check out work in Illinois, Maryland, and Wisconsin, just to name a few. Also, sign and share our letter to the ACLU asking them to join us in supporting safe and equitable access to healthcare. Sign on is open until 2/1/2024.
#op#covid#covid pandemic#covid news#covid 19#covid-19#covid isn't over#covid19#mask up#coronavirus#pandemic#people's cdc#pcdc#long covid#sars cov 2#sars-cov-2#coronavirus pandemic#wear a mask#covid variant#covid variants#covid vaccine#get vaccinated#covid vaccines#medical#disability#uspol#img#links#to read#described in alt text
187 notes
·
View notes
Text
COVID-19’s summer surge shows no signs of slowing down - Published Aug 17, 2024
Asurge in COVID-19 infections has swept the country this summer, upending travel plans and bringing fevers, coughs and general malaise. It shows no immediate sign of slowing.
While most of the country and the federal government has put the pandemic in the rearview mirror, the virus is mutating and new variants emerging.
Even though the Centers for Disease Control and Prevention (CDC) no longer tracks individual infection numbers, experts think it could be the biggest summer wave yet.
So far, the variants haven’t been proven to cause a more serious illness, and vaccines remain effective, but there’s no certainty about how the virus may yet change and what happens next.
The highest viral activity right now is in the West, according to wastewater data from the CDC, but a “high” or “very high” level of COVID-19 virus is being detected in wastewater in almost every state. And viral levels are much higher nationwide than they were this time last year and started increasing earlier in the summer.
Wastewater data is the most reliable method of tracking levels of viral activity because so few people test, but it can’t identify specific case numbers.
Part of the testing decline can be attributed to pandemic fatigue, but experts said it’s also an issue of access. Free at-home tests are increasingly hard to find. The government isn’t distributing them, and private insurance plans have not been required to cover them since the public health emergency ended in 2023.
COVID has spiked every summer since the start of the pandemic. Experts have said the surge is being driven by predictable trends like increased travel and extreme hot weather driving more people indoors, as well as by a trio of variants that account for nearly 70 percent of all infections. Vaccines and antivirals can blunt the worst of the virus, and hospital are no longer being overwhelmed like in the earliest days of the pandemic.
But there remains a sizeable number of people who are not up-to-date on vaccinations. There are concerns that diminished testing and low vaccination rates could make it easier for more dangerous variants to take hold.
“One of the things that’s distinctive about this summer is that the variants out there are extraordinarily contagious, so they’re spreading very, very widely, and lots of people are getting mild infections, many more than know it, because testing is way down,” said William Schaffner, a professor of preventive medicine and infectious diseases at Vanderbilt University.
That contagiousness means the virus is more likely to find the people most vulnerable — people over 65, people with certain preexisting conditions, or those who are immunocompromised.
In a July interview with the editor-in-chief of MedPage Today, the country’s former top infectious diseases doctor, Anthony Fauci, said people in high-risk categories need to take the virus seriously, even if the rest of the public does not.
“You don’t have to immobilize what you do and just cut yourself off from society,” Fauci said. “But regardless of what the current recommendations are, when you are in a crowded, closed space and you are an 85-year-old person with chronic lung disease or a 55-year-old person who’s morbidly obese with diabetes and hypertension, then you should be wearing a mask when you’re in closed indoor spaces.”
Schaffner said hospitalizations have been increasing in his region for at least the past five weeks, which surprised him.
“I thought probably they had peaked last week. Wrong. They went up again this week. So at least locally, we haven’t seen the peak yet. I would have expected this summer increase … to have plateaued and perhaps start to ease down. But we haven’t seen that yet,” he said.
Still, much of the country has moved on from the pandemic and is reacting to the surge with a collective shrug. COVID-19 is being treated like any other respiratory virus, including by the White House.
President Biden was infected in July. After isolating at home for several days and taking a course of the antiviral Paxlovid, he returned to campaign trial.
Biden is 81, meaning he’s considered high risk for severe infection. He received an updated coronavirus vaccine in September, but it’s not clear if he got a second one, which the CDC recommends for older Americans.
Updated vaccines that target the current variants are expected to be rolled out later this fall, and the CDC recommends everyone ages 6 months and older should receive one.
As of May, only 22.5 percent of adults in the United States reported having received the updated 2023-2024 vaccine that was released last fall and tailored to the XBB variant dominant at that time.
The immunity from older vaccines wanes over time, and while it doesn’t mean people are totally unprotected, Schaffner said, the most vulnerable should be cautious. Many people being infected now have significantly reduced immunity to the current mutated virus, but reduced immunity is better than no immunity.
People with healthy immune systems and who have previously been vaccinated or infected are still less likely to experience the more severe infections that result in hospitalization or death.
Almost “none of us are naive to COVID, but the people where the protection wanes the most are the most frail, the immunodeficient, the people with chronic underlying illnesses,” Schaffner said.
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#public health#wear a respirator
67 notes
·
View notes
Text
The U.S. is experiencing more than four times as many whooping cough cases compared with last year — a spike that some experts attribute to post-pandemic vaccine fatigue. “With the increase in vaccine hesitancy that has been going on since the Covid-19 pandemic, we’re seeing outbreaks occurring in kids who are not vaccinated,” said Dr. Tina Tan, president-elect of the Infectious Diseases Society of America. Babies are given the DTaP vaccine, which helps protect against three diseases: pertussis, diphtheria and tetanus. The vaccine works well against diphtheria and tetanus, but is less effective over time for pertussis. Advisors to the Food and Drug Administration met Friday to discuss the need for more robust and longer-lasting versions of the whooping cough vaccine. Until next generation vaccines are developed, boosters are recommended about every 10 years, starting in the tween years, as kids start middle school. It’s the tweens and teens whose immunity against whooping cough has waned that are driving outbreaks in many states, experts say.
26 notes
·
View notes
Text
Twice now I have tried to make a reblog reply about Walter and twice now Tumblr has eaten it. So let's try it this way @chaos-bringer-13
Allow me to take you back to the ✨QUARANTINE DAYS✨ and tell you the tale of a pumpkin that may or may not have housed a god
So back in good old 2020/21 we are in the thrall of the COVID-19 pandemic. My state in particular had super heavy quarantine restrictions, and as someone with lung issues, my mom and myself were not taking any chances. I haven't left my house in maybe 5 months. Nor have I seen any of my friends outside of video calls. Senior year of High School so far has sucked.
I'm talking to my friend, we'll call her Marie, and I mention off hand "Yeah I'm starting to feel a bit lonely." Now Marie has known me for a solid 8 years at this point. She knows my type of humor and attachment to what we would now and days call "skrungly" objects. She decides "hmm. I can fix this!"
Marie's mom (who was... certainly a human being) for some god forsaken reason decided to buy a white pumpkin and give it to Marie with the idea that she would harvest the seeds from it and plant them in the garden (why she did this instead of just buying pumpkin seeds I will never know). Instead of doing this, Marie takes this pumpkin and draws a realistic face on it that can only be described as similar to the handsome squidward meme. She drives to my house, sets the pumpkin on my doorstep with a note, and then FUCKING BOOKS IT.
I open the door to see this pumpkin with a note that reads "Hello Momther, I am Walter."

(Not the best photo but this is in fact Walter sitting in the dark in my front yard while Marie (not pictured) stands on my driveway holding a single candle and chanting).
Anyway immediately I take him inside completely smitten and unknowing as to what this pumpkin will create.
At this point of quarantine, we have gone back to classes but they are completely online. I decide that the best thing I could possibly do with Walter is set him on a stack of notebooks behind me so that when I turn my camera on he would be there... watching. Notably, one guy who never unmuted himself did so just long enough to ask "Void... what the fuck is that."
Needless to say I got endless entertainment from the reactions, but all good things have to come to an end. Unfortunately, I live in a desert and pumpkins simply don't survive. They typically would rot within a few days where I was living at the time, so my Mom told me to move it outside at least. I decide to put him by the front door. This front door has a little half wall that leads up to it. I put him on top of it facing the walkway so whenever a package is delivered the mailman would be faced with Walter and have to make eye contact before leaving the mail. I figure I'll probably get a couple more days out of him before he rots.
This is where it starts to get weird
Another week passes. Two. Unlike every single pumpkin I've ever had for Halloween, Walter shows no signs of rotting despite being exposed to the elements. The pumpkin is at this point about a month and a half old and still perfectly fine. Marie, our friends, and I all kind of laugh it off as a random one time thing and expect it to rot within another week.
IT. FUCKING. DOESN'T.
4 months into having Walter and he is still as good as new. Around this time the vaccines for covid started rolling out, so my friends and I get to see each other again. They are just as baffled as me about Walter. Of course, us being us, we have been referring to Walter like an actual person this whole time because that's just our humor. We give him little head pats and forehead rubs as we enter or leave my house and say hello/goodbye to him.
Also around this time, my mom and myself are beginning to prep for moving to another state. We have also started doing some in person classes again. I had been cleaning out my room one morning, and just so happened to leave a piece of sea glass in front of Walter as I left for school. I had a strangely good day. Managed to get an A on a test if I remember right. I come home, see the glass in front of the pumpkin, and start thinking. The next day I leave him something else. Another good luck day! I try this again and every single time I leave him an offering something good happens! I tell my friends about it and they start doing it too and experiencing the same results. We decide that he must be some god of luck inhabiting this pumpkin vessel and rewinding time on it to keep it from rotting.
At some point someone gave him an orange and I swear to god the pumpkin started getting orange marks on its forehead. He still wasn't rotting though! We decided that he obviously has been absorbing the power from the offerings.
Around this time I realise the I have somehow created a partially serious cult and decide I might as well lean into it. I actually enlisted the help of the neighbor kids to take this photo.

Time passes. Walter is about 10 months old now and still going strong. We have graduated highschool and I'm going to be moving in a week. I can't take Walter with me, so Marie decides she will take him. But first, she is going to help us move. It's a 6 hour drive. We put Walter in the passenger seat window so that all the cars passing us can see him.

After she helps us, Marie and Walter continue on to yet another state where Marie will be attending university. Walter is almost if not a year old when he finally starts to rot. Marie, in her dorm room mind you, makes a plaster cast of his head and redraws his face on it. To this day Walter hangs in his new, more durable vessel, guarding her spice cabinet.

By the end of Walter's reign, he had reached his 1st birthday, scared who knows how many mailmen, met 3 of my teachers in person, visited 3 USA states, and briefly had an instagram account.
#im pretty sure it was the heat of the car that finally kickstarted him to rot#he also used to bless things#like we buried a jar in the front yard full of modified plastic forks (we made fork denominations)#we had him bless that place we buried it by lighting a candle ominously in front of his face and simba-ing him with mint#walter the immortal
29 notes
·
View notes
Note
Hi! I'm a longtime kaylor lurker, but I saw you and your anons were trying to think through the reason for this Travis Kelce push and I thought I'd share some perspective as an American who's not exactly a football fan per se, but is from an area of the country where football is very popular so I'm kind of an ambient fan by default. I'm very sorry this got a little long, but I do think there are some really interesting dynamics at play here, but the tldr; is - broad appeal for the American premiere and politics.
There are some optics about Travis Kelce that are I think getting lost in the NFL-to-Swiftie translation that may be important. He's a famous football player, yes, but NFL fans skew heavily towards older men in non-urban areas, which also means NFL fans skew conservative. Travis Kelce promoted Bud Light when transphobes in America were boycotting the brand, and is also partnering with Pfizer for a public health campaign to promote the COVID-19 vaccine, which is very controversial for American conservatives. He's also known as a very stylish man (which is weird to say but is pretty uncommon among American athletes, especially white ones, and he's well-known for it) and before Taylor, all of his known/rumored exes have been Black or mixed (I could write an essay on the racial dynamics alone of this weekend, but... suffice it to say it's there and messy). I'd also heard rumors that he was closeted before he got together with Taylor, but I never really looked into them that deeply so I don't know how true they are, or whether they arose just because he dresses well and doesn't usually date white women (sad but true that for a portion of Americans, that would be enough to make them doubt his masculinity and therefore heterosexuality). Which kind of gets to my point - before this, a lot of the more conservative wing of NFL fans saw Travis Kelce as controversial, "beta", not sufficiently manly, despite the fact he is a champion football player. I know all of this sounds a little insane, please remember that these are the people electing Donald Trump and going after drag shows and banning books with LGBTQ+ people in them.
So, with that slightly more nuanced image of Travis Kelce, I think that makes the clearest takeaway from this weekend, at least for me, how extremely traditional all-American it was. Football player, blonde girl cheering in the stands with his mom, driving off in his convertible after the game, them making a point to correct the initial reporting that she had paid for people's meals so that he's the one renting out the restaurant for her. To be clear, this isn't really how Travis Kelce is normally seen, and already I've seen some hit tweets with people dunking on conservatives criticizing Kelce for being insufficiently manly by responding something along the lines of "uh, he won the Super Bowl and bagged the world's most famous pop star, I think he's doing okay" - so, reading between the lines, he's performed (specifically) white masculinity very successfully. And for Taylor, too, I think we've already seen a lot of people saying how she's finally with a "real man" - he's very tall, he's very athletic, he's American, I think a lot of the joking anti-Joe "he's got a real job" comments fall into this bucket as well. She is performing white American womanhood in a very specific way, a large part of which is that she's being framed as not the 'dominant' partner in the relationship in the way she was in her relationship with Joe (by virtue of their differences in wealth and success).
So I think this is re-orienting both of their images into a new, very traditional, Americana-inspired direction. I don't think this is a market Taylor has really gone after maybe since she moved into pop in the first place, but especially not in recent years, when she swung very hard into a much more urban liberal niche (basing herself more out of NYC and London than Nashville, associating herself musically and socially with people like the Haim sisters, Phoebe Bridgers, MUNA).
I don't think we can know exactly why she's leaning this direction yet, but if I had to guess it's more about the American documentary premiere. In Hollywood, typically for the biggest box office impact you want a "four-quadrant movie" - one that appeals to the four biggest demographic quadrants (male/female and under 25/over 25). Taylor Swift's fanbase skews female and young, with a solid presence over 25 as well, and like I said earlier, the NFL's fanbase skews male and over 25. I don't think showing up to a football game will make a bunch of NFL fans suddenly want to see her documentary on opening night, but it may make them more inclined to go see it with their girlfriends, wives, or daughters a few days later, instead of staying at home, and that would have a very big box office impact.
I also think she *might* be looking at the political optics, and wanting to not only move on from MH but also put herself in a kind of solidly centrist-liberal place (she likes good ol' American football but also the vaccine! she votes Dem but she's not one of those New York liberal elites, she eats chicken tenders with seemingly ranch! - truly seems like this is a couple tailor-made (or maybe Taylor-made ;) ) to appeal to swing voters), which I think is very much where she tried to position herself with Miss Americana as well and which seems relevant given her voter registration push recently and as we move into an election year. I'll be very interested to see if she does anything further politically, or says anything about politics in her documentary again. Between her voter registration effort and his Pfizer partnership and the timing of both, politics is actually the angle I'd bet on driving this.
hi! thank you for sharing these thoughts, it provides more context for everything! i do think it shapes her persona in the public eye, and it’s interesting to think how that might benefit her in ways other than a profit motivation
56 notes
·
View notes
Text
Batman vs COVID-19
Batman's strengths:
He has experience from Contagion/Legacy
He probably has access to high quality masks
He probably would have been able to make his own vaccine (this would not prevent him from getting it, it would just make it so his symptoms aren't as bad)
Batman's weaknesses:
Even if he had access to masks, he might not use them (as seen in Contagion and Legacy)
He has an unrelenting drive to fight crime (puts him in close contact with a lot of people)
Feel free to make your case!!
9 notes
·
View notes
Text
By Peter A. McCullough, MD, MPH
For years, my younger followers have been concerned over the COVID-19 vaccine, dating, and sex. Such concerns have been the driving force behind the dating site Unjected.com. Recently, SARS-CoV-2 virions have been found in sperm months after COVID-19 infection.
In 2023, Chillon et al found anti-SARS-CoV-2 Spike antibodies in semen of 43 vaccinated (mainly Pfizer and Moderna) and 43 matched, unvaccinated men. They found the antibodies correlated with plasma concentrations and the number of vaccine shots taken (at 3/4 shots all mRNA products). The unvaccinated had antibodies to SARS-CoV-2 from the natural infection, however the concentrations were many log-fold lower than the vaccinated. The authors found no differences in sperm quality between the two groups.
5 notes
·
View notes
Text
Six weeks after Li Wenliang blew the whistle in Wuhan on an emerging infectious disease in early 2020, cities around the world locked down and turned into hotspots. From Rome to Tokyo to San Francisco and Los Angeles, COVID-19 ripped through the most populated areas of the world. By the end of that year, America’s cities—Detroit, Boston, and New Orleans among them—had death rates from the virus 20 percent higher than other regions of the country.
In New York, where I serve as health commissioner, almost 50,000 residents died, the majority in the first three months, denting New Yorkers’ life expectancy by nearly five years. It was the steepest drop in lifespan in the world that year.
Public health institutions and the field as a whole learned much from our successes and failures during the pandemic. The critical nature of healthcare supply chains; supporting our public health workforce, especially at the front lines; the essential process of community engagement for healthcare promotion, vaccination, and disease prevention; the importance of combatting misinformation and disinformation online and in person; the need to tear down our data silos so we can make faster, better decisions. The list goes on and on.
However, as new threats arise and old ones intensify, there is still much to learn. Cities—concrete jungles that experienced the worst of COVID-19, and in some ways, struggled the most with the public health response in the early days of the pandemic—may be our best teachers on how to keep our world safe and healthy.
That’s because the sentinel cases for brooding public health threats, whether infectious or not, are often in cities. Cities are the canaries in the public health coal mine, for everything from mental health and homelessness, climate change to forced migration, substance use to sex trafficking. The way these challenges play out across our cities should not only drive national policy, but also serve as an important corollary for how to respond in less dense, less diverse, more rural areas. Yet when we consider the multilateral institutions where decisions are made and policymaking happens, cities rarely have any role in governance.
The reasons for city-as-public-health-epicenter are simultaneously obvious and not so obvious. For one, urban densification has accounted for the majority of population growth, even as land mass occupied by cities is growing. Today, around 56 percent of the world’s population live in cities—a percentage that experts expect will grow to 70 percent, with population doubling, by 2050. There is also the historic boom in airplane travel both domestically and internationally, which means communicable diseases (like SARS, swine flu, and mpox) can leap across borders faster than ever, quickly overtaking cities’ health systems.
An example of this in New York City in 2022 was when an old virus, mpox (formerly known as monkeypox), began circulating in explosive new ways among men who have sex with men. NYC had become the national and global epicenter.
Despite facing critical shortages of vaccine, in June 2022 we began vaccinating men who had the highest risk of getting infected, well ahead of the anyone else in the nation, including the federal government. This critical intervention to curb the virus’s spread helped bend the curve of mpox within a few weeks, by early August. Not only did our response set the tone for the rest of the national mpox response, it also influenced the way in which many other global centers responded.
The same happened with tuberculosis (TB), another old microbe—and one that remains a leading infectious killer in the world. Between 2022 and 2023, the U.S. has seen a dramatic 14 percent year-on-year increase in tuberculosis cases nationwide. NYC is once again at the country’s frontlines, with a 28 percent increase over the same period. The drivers of TB’s resurgence are manifold, but one is the shifting pattern of migration worldwide due to climate change, war, and economic and political instability.
NYC health officials again leapt into action. We not only increased investment into our TB program in response, but since 2014 have pioneered new and effective ways to control the disease including award-winning “video directly observed therapy” where a health worker observes the patient taking their daily medications. This telehealth protocol has now become a part of TB control guidance recommended by the World Health Organization.
But while cities like New York are battling disease threats with drive and innovation, a lack of formal representation in multilateral institutions means that cities are more susceptible to security concerns, bioterrorism, and economic disruption. Cities are largely expected to navigate their response to global health crises in silos, without a clear and dedicated means to exchange ideas between them. Moreover, they typically do not have a meaningful say in how their national counterparts navigate domestic responses or global deliberations.
That was New York City’s early experience during the pandemic.
As COVID-19 tore through our five boroughs in the early weeks and months—from Sheepshead Bay and Jamaica to Battery Park, Harlem and Hunts Point—New York’s public health authorities produced their own messaging campaigns; partnered with private corporations and others to source materials and protective equipment for healthcare workers to care for those in need; stood up a free testing network, and later; designed their own vaccine distribution system and engaged deeply with communities to promote vaccine uptake. These responses were—especially early in the pandemic—developed in the absence of clear national and international guidance, or resources. And our experience in the start-up phase of the pandemic response was not unique, with cities from Los Angeles to Chicago to Boston to Miami facing similar challenges.
If we don’t formally involve cities in our national systems for disease surveillance and public health response, we lose out. Best practices disappear into the archives. Innovative strategies collect dust in the pages of textbooks and journals. How can cities effectively respond to burgeoning health threats when institutional memory fades, and when protocols developed at national scale lack the specificity or practicality to actualize in our alleys or on our sidewalks?
A better strategy may pull from the discipline of political science: specifically, a concept known as “inclusive multilateralism.” This concept, which refers to the participation of non-nation states in multilateral institutions and processes, narrows the gap between the high-level authorities handing down policy decisions and the communities on the ground who are expected to make them come to life. It has allowed for civil society, nongovernmental organizations, the private sector, and other stakeholders to have a formal role in the most critical multilateral governance structures in the world, from international security to climate change bodies. It also creates a critical set of checks and balances, ensuring that special interests or anti-democratic actors, influencing national governments and elected leaders, do not have outsized sway in international decision-making by having representation of sectors outside of national politics.
In health, for instance, the Global Fund to Fight AIDS, TB, and malaria, among others, have since inception had official civil society and private sector representation on its governing board and country coordinating bodies.
There is a growing appetite for cities to have such a formal leadership role, not only to share local experiences, best practices, innovations, and data, but also to build collaborations for emergencies. In remarks made during an event honoring the United Nations’ 75th Anniversary in 2020, Secretary General António Guterres specifically called out the need to draw on the “critical contributions” of cities and regional governments. Similarly, the 2017 Partnership for Healthy Cities launch stated that “city leaders are uniquely positioned to drive policies and programs to help transform public health. And a recent McKinsey report suggests sizable potential impact through a global focus on city-level work, not just for pandemic preparedness, but for overall health. They estimate that influenceable interventions at the city level could add more than 20 billion years of higher-quality life at a global level, while offering a critical opportunity to address health disparities and inequities, an important underlying driver of differential outcomes from pandemic disease, let alone chronic health challenges.
Following these leads, it is time national governments and multi-national organizations formalize the role of cities in global health governance and security. One proposal is that relevant multilateral institutions—such as the World Health Organization or World Bank—could establish seats for cities on their Executive Boards or Board Committees. These seats could even have city government representation from both donor and implementer countries. Additionally, each region could add representation for cities on their subcommittees or local oversight bodies, for example U.N. Country Offices or Country Coordinating Mechanisms.
Now, as the global health community gathers this week in Geneva for the World Health Assembly – the annual gathering of the official governing body of the WHO—there is an opportunity ripe for the inclusion of the local jurisdictions who will be at the forefront of the next pandemic. Negotiations on the Pandemic Accord, the global treaty intended to set international standards of preparedness, cooperation, and communication between nations in advance of the next global communicable disease threat, are set to conclude this week. It is essential that real-world lessons and insights from cities are incorporated into this document, to ensure well-meaning agreements translate to real-world action on the ground.
There are already glimmers of hope.
In the last two years, Tedros Ghebreyesus, director-general of the WHO, has invited New York City to attend the annual World Health Assembly, the official decision-making body for the WHO and the International Health Regulations. That inclusion has allowed us to share our hard-won experience with WHO and other officials, in regard to the forthcoming Pandemic accord, including our insights on building stockpiles of PPE, mobilizing the health workforce and managing health facility capacity, ramping up testing through public-private partnerships with commercial laboratories, building a rapid and locally-driven vaccination effort, and ensuring that equity and place-based work is incorporated at the start of a response, rather than in subsequent phases. And in return, we learned first-hand about many of the challenges faced by nations across the globe in pandemic response and disease surveillance, especially in light of a changing climate and critical health workforce shortages, and have incorporated learnings about the WHO’s data sharing capacities and early warning and advanced surveillance systems, into improving our own population health data system.
New York City’s presence at the World Health Assembly has also given us an opportunity to demonstrate our front-line expertise and innovation in mental health, urban preparedness, climate change adaption, data modernization, and emerging health issues related to the global migrant crisis, among other issues.
Designing formal mechanisms to include cities in deliberations of global scale will allow each of us to not only sound the alarm earlier, but also to better respond to emerging public health threats lurking in our streets and sewers. By ensuring that cities have a meaningful seat at the table in our global health governance models, we will be charting a better course for the world to respond to forthcoming crises.
13 notes
·
View notes
Text
Even with a new booster, the XBB.1.5 vaccine offered no increased protection from infection against the JN.1 variant. This alarming discovery underscores the virus's relentless ability to mutate and evade our defenses, fueling continued transmission, evolution, and the devastating threat of Long COVID.
"Ongoing evolution of SARS-CoV-2 drives escape from mRNA vaccine-induced humoral immunity"
(March 07, 2024)
"However, progressive loss of neutralization was observed across newer variants, irrespective of vaccine doses. Importantly, an updated XBB.1.5 booster significantly increased titers against newer variants but not JN.1. These findings demonstrate that seasonal boosters improve titers against contemporaneous strains, but novel variants continue to evade updated mRNA vaccines, demonstrating the need for novel approaches to adequately control SARS-CoV-2 transmission."
17 notes
·
View notes
Text
The FDA, between now and May 8, is accepting public comments for their upcoming vaccine committee meeting. Let them know that all of us need access to COVID vaccines at least twice a year.
Make your voice heard and ask the FDA Vaccines and Related Biological Products Advisory Committee Meeting to:
Ensure vaccine manufacturers anticipate the upcoming dominant strain of SARS-CoV-2.
Recommend updated COVID vaccines for all ages AND
Strengthen our vaccine drive by recommending more frequent boosting (at least every six months) and more frequent updates to the vaccines, adjusted for the latest variants.
Submit a public comment. Feel free to use our sample language below.
You can also register to give Oral Public Comment at the upcoming May 16 online FDA Vaccines and Related Biological Products Advisory Committee Meeting at: [email protected] on May 1, 2024. THAT’S TONIGHT!
Submitted written comments for the meeting must be received by the FDA via the Federal Register no later than May 8, 2024 at 11:59 Eastern Daylight Time.
It’s important to submit a personalized comment, which could include the importance of anticipating the next dominant viral strain, the lack of vaccine access that has impacted or would impact you, or how out-of-pocket costs are a barrier in your family or community. Feel free to take inspiration from or borrow the language in our sample public comment below.
Docket No. FDA–2024–N–0970 Scientific evidence indicates updated vaccines are needed to address the ongoing changes in COVID variants, and they should ideally be allowed, available, and fully covered by public funds and/or insurance, for people of all ages at least every six months. The vaccine schedule should address waning efficacy in the months following vaccination [1-3] as well as emergence of new SARS-CoV-2 strains. The FDA’s decision will affect the current and future vaccine approach including what healthcare providers recommend, what health insurance covers, and level of public engagement. It is of utmost importance that the FDA anticipates the newest viral variants and provides recommendations that anticipates the next dominant strain in the next six months. This requires that the FDA ensure that manufacturers anticipate the newest variants. Restricting vaccinations to only annual updates misses an opportunity, given that there is the potential to update the vaccines to better match perpetually emerging variants. Updates to all vaccine types are needed, and mRNA vaccines are particularly suited to frequent updates. The recommendation for only annual vaccination also creates barriers for vulnerable people and discourages high risk people from getting needed vaccine boosters. The FDA must ensure support equitable and affordable access to updated vaccines and prevent limited access because of financial constraints or demographics by advocating for programs such as the CDC’s bridge program that ensures no cost access. [4] References:
Link-Gelles R. COVID-19 vaccine effectiveness updates. Presented at: FDA VRBPAC Meeting; June 15, 2023. Accessed February 9, 2024. https://www.fda.gov/media/169536/download
Wu N, Joyal-Desmarais K, Vieira AM, et al. COVID-19 boosters versus primary series: update to a living review. The Lancet Respiratory Medicine. 2023;11(10):e87-e88. doi:10.1016/S2213-2600(23)00265-5
Menegale F, Manica M, Zardini A, et al. Evaluation of Waning of SARS-CoV-2 Vaccine–Induced Immunity: A Systematic Review and Meta-analysis. JAMA Netw Open. 2023;6(5):e2310650. doi:10.1001/jamanetworkopen.2023.10650
https://www.cdc.gov/vaccines/programs/bridge/index.html
Full instructions for written and oral comment and meeting information can be found at: https://www.fda.gov/advisory-committees/advisory-committee-calendar/vaccines-and-related-biological-products-advisory-committee-may-16-2024-meeting-announcement
FDA Vaccines and Related Biological Products Advisory Committee Meeting on the Federal Register: https://www.federalregister.gov/documents/2024/03/04/2024-04523/vaccines-and-related-biological-products-advisory-committee-notice-of-meeting-establishment-of-a
#op#uspol#medical#public health#covid#covid-19#covid19#covid 19#coronavirus#sars-cov-2#sars cov 2#pandemic#coronavirus pandemic#covid pandemic#covid vaccine#covid conscious#covid cautious#covid isn't over#food and drug administration#fda#people's cdc#pcdc#links
13 notes
·
View notes
Text
also preserved on our archive
By Korin Miller
Many COVID-19 variants have come and gone since the pandemic began, but some get more buzz than others. Now, there’s another new variant getting attention from the infectious disease community. It’s called XEC, and it’s currently spreading in Europe.
XEC is an Omicron variant that descended from subvariants KS.1.1 and FLiRT variant KP.3.3, according to Scripps Research’s Outbreak.info. XEC has several spike mutations, which is what the virus uses to infect you—and it might be more infectious that previous strains because of it.
So, will the new variant hit the U.S.? What symptoms should be on your radar? Here’s the deal.
Meet the experts: Amy Edwards, MD, associate professor at Case Western Reserve University and director of the Pediatric COVID Recovery Clinic at UH Rainbow Babies and Children’s Hospital; Mark Cameron, PhD, an associate professor in the Department of Population and Quantitative Health Sciences at the Case Western Reserve University School of Medicine. Emily Smith, ScD, MPH, is an epidemiologist and an assistant professor at the George Washington University Milken Institute School of Public Health.
What symptoms should I watch for? XEC is a pretty new variant and, with that, there isn’t a ton of information right now on symptoms people have experienced with it. However, early reports don’t suggest that it causes dramatically different symptoms from other strains of COVID-19.
According to the Centers for Disease Control and Prevention (CDC), symptoms may include:
Fever or chills
Cough
Shortness of breath or difficulty breathing
Sore throat
Congestion or runny nose
New loss of taste or smell
Fatigue
Muscle or body aches
Headache
Nausea or vomiting
Diarrhea
When will the new variant hit the U.S.? While the XEC variant is getting a lot of attention in Europe, it’s already hit the U.S. As of Sept. 3, data show that there have been 23 cases of COVID-19 caused by the XEC variant in the U.S., with three happening in California.
The virus was first detected here on July 14, but hasn’t been detected since Aug. 16. That doesn’t mean it’s no longer here, though. Because so many people do home tests (or don’t test at all) when they have symptoms of COVID-19, it can be tricky to get information on different strains of COVID-19.
Will it become the dominant COVID variant? That’s not clear. As of this second, XEC isn’t even a blip on the CDC’s radar. The CDC’s variant surveillance system shows that KP.3.1.1 is the dominant strain in the U.S., followed by KP.2.3, and LB.1. XEC isn’t even listed on the surveillance.
That doesn’t mean it won’t spread, though.
“Just like JN.1 emerged from BA.2.86 late last year to drive new COVID infections through last fall and winter, XEC may have similar potential,” says Mark Cameron, PhD, an associate professor in the Department of Population and Quantitative Health Sciences at the Case Western Reserve University School of Medicine. “But we need to know more about the XEC variant and perhaps those still to come.”
But lately we’ve seen several variants circulate heavily at the same time, points out Amy Edwards, MD, associate professor at Case Western Reserve University and director of the Pediatric COVID Recovery Clinic at UH Rainbow Babies and Children’s Hospital. “Dominant is a strong word,” she says. “With so many very contagious variants, I think the days of having one dominant variant is gone.”
How can I protect myself? The CDC currently recommends that everyone aged 6 months and up get the updated COVID-19 vaccine, making that a good place to start. “As yet another Omicron family member, being up to date on the latest COVID-19 booster is a protective measure we can take right now,” Cameron says.
"The main thing we can do to slow a new variant or new wave is to get our booster shots this fall," says Emily Smith, ScD, MPH, an epidemiologist and an assistant professor at the George Washington University Milken Institute School of Public Health. "Generally, we find the boosters give us broad protection, even against new variants."
It’s also a good idea to wear a mask in crowded indoor areas when levels of COVID-19 are high in your area, especially if you’re consider high risk for complications of the virus. And, of course, if you develop symptoms of the virus, it’s a good idea to test yourself to see if you have the virus so you can lower the odds you’ll spread it to others.
If you do, in fact, have COVID-19 and are considered high risk for serious complications from the virus, you may want to contact your primary care physician about taking an antiviral medication like Paxlovid.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator
39 notes
·
View notes
Text
COVID-19
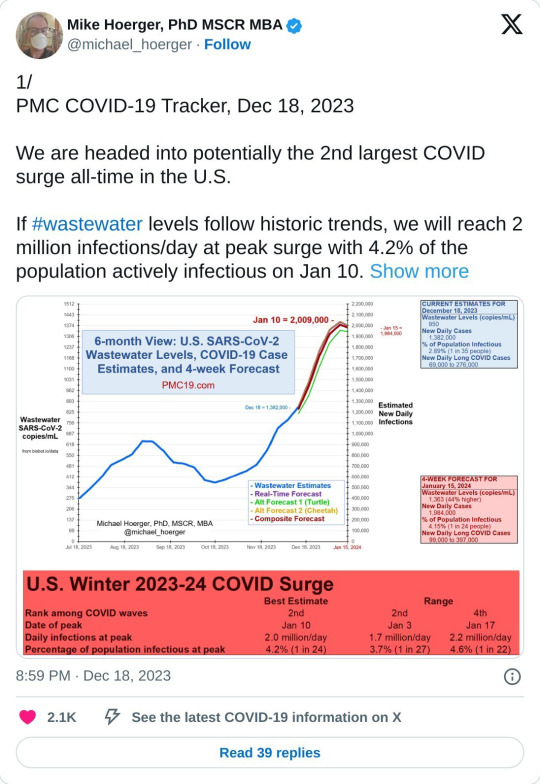
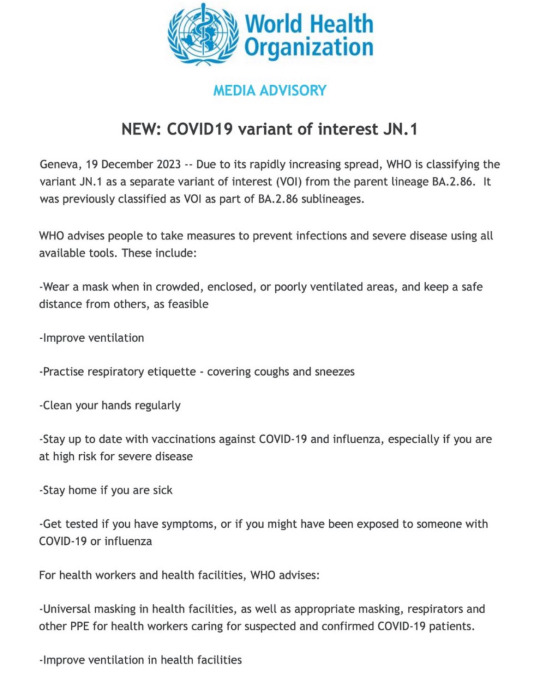
We are currently in the largest COVID surge of all-time in the US.
There is also a new variant that is not protected by the previous vaccine.
Please start back masking and please get the COVID-19 booster (schedule with your local pharmacy).
Wastewater counts are obscenely high right now, belying the official case numbers. Considering that we've stopped collecting or reporting most COVID data, wastewater is the best way we have to judge the actual infection rate now. Wastewater is collected from washing our hands, going the bathroom, etc. We shed COVID into the water system and based on the concentration of COVID in waste water, we can get very accurate estimates of how many people are infected at one time.
We are currently seeing ten million new infections a week, and can expect that to greatly increase within the next three weeks.
* If you've stopped masking, please start again, for your own safety and the safety of your community. Many hospital systems are already trending toward being overwhelmed right now; wear a mask when in crowded, enclosed, or poorly ventilated areas, and keep a safe distance from others, as feasible.
* Avoid unnecessary gatherings where possible.
* Ventilate your spaces well (Corsi-Rosenthal Box).
* Reevaluate casual habits (touching face, respiratory etiquette—covering coughs and sneezes, clean your hands regularly, stay home if you are sick, get tested if you have symptoms, or if you might have been exposed to someone with COVID-19 or influenza)
Please be aware of Long Covid.
COVID impacts the immune system similar to HIV in that it hides in the body and continues to wreak havoc in the various organ system by driving inflammation and disrupting the immune response. It causes neurological, vascular, and immune dysfunction.
Patients with long COVID generally have symptoms that fall into three categories or phenotypes: fatigue, neurocognitive symptoms such as brain fog or headaches, and cardiovascular symptoms such as shortness of breath, heart arrythmias, exercise intolerance, and blood clots. Patients may have more than one type, and some also have symptoms like constipation, diarrhea, or loss of taste and smell that don’t seem to fit neatly into one of the three groups.
This is a period where we need to act with more care. Not a time to panic, but a time to be more cautious.
If you contract COVID, these are some helpful things that work to reduce viral load in the hope of minimising symptoms. And your chance of developing Long Covid:
* Brush & floss as usual
* Mouthwash (CPC (cetylpyridinium chloride, an ingredient in many/most commercial mouthwashes), cooled green tea, salt water)
* Green Tea (drink on an empty stomach if possible; can also be used for swishing/gargling once it has cooled; if green tea isn't doable for you, black tea is an alternative)
* Nasal Spray (if chemicals in nasal spray causing an issue for you, saline nasal spray also an option)
* Vitamin C supplement
* Antihistamines
* Other prophylactics to consider: Nattokinase, Grape Seed Extract, EGCG supplements
* Natto (if this is something you already eat, or would like to try. It's fermented soya beans and is popular in Japan
* Mask & Vaccinate!! A fully vaccinated individual is five times less likely to continue to have any symptoms or ill-effects three months after their initial infection compared to someone who has not been vaccinated.
Not a medical professional but compiled resources from medical professionals and individuals with disabilities including long COVID.
Free Palestine. Free Congo. Free Sudan. Free Tigray. Stop Cop City. Eyes on the Mass Graves in Jackson.
Please SHARE & Please participate in the Global Strike for Palestine 1.21-1.28.
#covid#covid19#long covid#covid isn't over#covid 19#coronavirus#corona#free palestine#free gaza#free congo#free sudan#freepalastine🇵🇸#freedom#black liberation#israel is committing genocide#israel is a terrorist state#end occupation#human rights#hawai'i#land back#decolonization#nakba#jason todd x reader#free tigray#stopcopcity#copcity#congo genocide#save congo#mass graves in jackson#jackson mississippi
14 notes
·
View notes
Text
The Impact of COVID-19 on Healthcare Systems
Written by Dev
The COVID-19 pandemic hit healthcare systems worldwide, exposing serious weaknesses and forcing rapid changes. Hospitals were overwhelmed with patients, leading to shortages of beds, oxygen, and protective gear. In places like India, where the healthcare system was already under pressure, these shortages were especially severe, with many patients struggling to get care.
As hospitals focused on treating COVID-19, many regular services like surgeries, cancer treatments, and vaccinations were delayed or canceled. This led to other health issues, like an increase in maternal and child deaths due to lack of access to basic care. For children, interrupted vaccination programs risked future outbreaks of preventable diseases, making this health crisis even worse in the long run. Additionally, multiple countries lacked the proper monetary resources and funding to effectively handle this disaster, aggravating the strain on resources, since the ones that were able to receive healthcare were receiving the same in poor quality, leading to occasional incomplete treatments of the same.
Since all medical resources went towards Covid-19 patients, there was a strain on treating other diseases like Cancer, multiple STDs, etc. Additionally, the lockdown also prevented routine check-ups, leading to a surge in patients with worsening conditions, not necessarily involved with Covid-19. The frequent postponing of health check-ups caused multiple disadvantages, and is a variable that could have lessened the load on the healthcare system.
The pandemic also triggered a disturbing rise in attacks on healthcare workers. According to the World Health Organization (WHO), healthcare staff worldwide faced violence, abuse, and stigma. In many cases, healthcare workers were wrongly seen as “spreaders” of COVID-19, leading to harassment and even physical assault. This fear and misinformation affected not only healthcare workers’ safety but also made it harder to provide medical care.
Mental health issues increased during the pandemic too. Many healthcare workers struggled with stress, burnout, and trauma due to high patient death rates and long hours. The importance for mental health was severely underscored during the time of the pandemic, considering extreme levels of anxiety between not only patients but also regular people. People outside the healthcare field also faced mental health challenges from lockdowns, isolation, and fear of infection. With demand for mental health services rising, healthcare systems struggled to keep up. Health scares combined with break in routine spread widespread paranoia within the people.
However, the crisis did lead to some useful changes, like the growth of telemedicine, which allowed patients to talk to doctors remotely. This made it easier for people to get healthcare without leaving their homes and helped hospitals reduce patient crowding. Many healthcare providers also set up drive-through testing and vaccination centers to make these services more accessible. These new methods of delivering healthcare might continue to improve access even after the pandemic.
Additionally, it introduced newever, more enhanced protocols when faced with death or serious situations, which only improved time and response of healthcare systems. The anxiety and mental stress caused by the pandemic also increased the availability of mental health resources and help to people, a part that helped reduced the stigma surrounding mental health.
COVID-19 has shown that healthcare systems need to be stronger and more flexible to handle future crises. Governments and healthcare leaders are encouraged to invest more in public health, improve safety protections for healthcare workers, and support mental health resources. By learning from COVID-19, healthcare systems can better protect both patients and providers when the next crisis comes.
#covicare#covid#covid 19#group#health#post covid#awareness#mental health#team#wellbeing#article#blog#healthcare system#healthcare
4 notes
·
View notes